Tuberculosis has now surpassed COVID-19 and reclaimed its spot as the world’s most deadly infectious disease. With 8.2 million people newly diagnosed with TB in 2023, these latest figures reflect the highest number of global cases since the WHO began monitoring in 1995. While the risk in the U.S. is considered to be very low and the number of cases is significantly lower, cases have increased. In 2023 cases rose by 16% over 2022, marking the highest number (9,615) in the U.S. since 2013 (9,556). On a more positive note, the estimated number of global TB deaths decreased in 2023 (1.25 million) from 2022 (1.32 million).
According to the WHO Global Tuberculosis Report 2024, low- and middle-income countries bear 98% of the disease burden, with 56% of all illnesses in India (26%), Indonesia (10%), China (6.8%), the Philippines (6.8%), and Pakistan (6.3%). While the report noted that much of the global increase likely reflects population growth, global funding for TB prevention and care has decreased and is well below target levels.
One significant issue in prevention and care is the multidrug resistance of TB and length, and thereby costs, of treatment needed. In fact, treatment for active TB disease can take months or years, with treatment plans including different combinations of medicines. Thus, treatment is complex, requiring a TB medical expert.
Another issue is that a person can have TB and have no symptoms, a condition called inactive or latent TB infection – with the CDC estimating that up to 13 million people in the US live with inactive TB. While these persons cannot spread the disease, without treatment their condition can develop into active TB at any time. Because of this, anyone who has been exposed to TB should be tested, and, if positive, should start treatment to protect against illness.
Because TB is an infectious disease, and the course of treatment is long and costly, businesses should ensure their workforce understand the symptoms (e.g., cough, chest pain, fever, chills, fatigue, shortness of breath, coughing up blood or sputum [phlegm]), and are able to receive adequate treatment. Not only can lack of treatment increase the spread of the disease, stopping treatment before the full course is run can generate more drug-resistant cases.
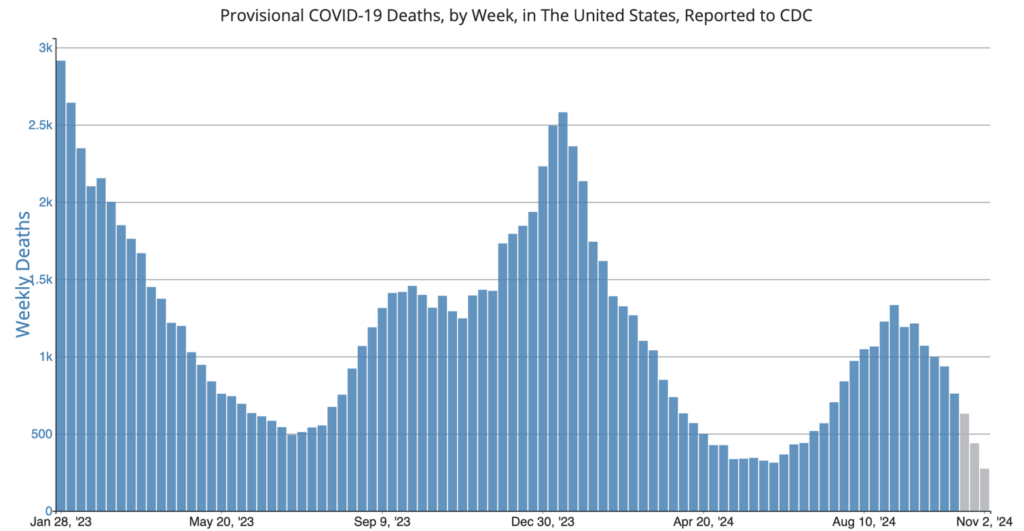
COVID Risk Matrix:
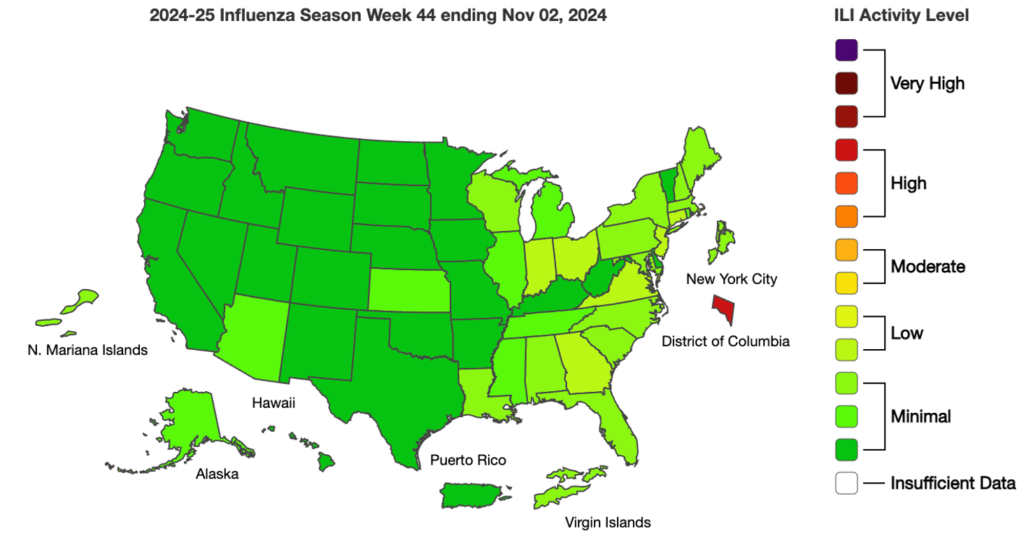
Influenza:
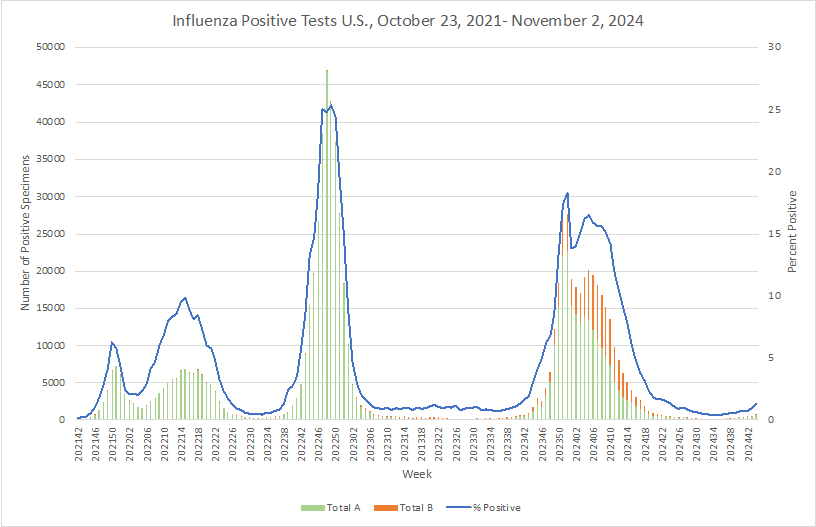
- The CDC published a piece about flu hospitalization trends from 2010- 2023. The majority of hospitalizations occur in people aged 65 and over with underlying health conditions including hypertension, obesity, and various chronic conditions. Antiviral use decreased during the study time period. The use of molecular assays, particularly multiplex standard molecular assays, used for detection of influenza has increased to be the main method for identification of cases.
- A placebo-controlled study of 335 persons compared simultaneous administration of the COVID-19 and influenza vaccines with those given sequentially 1-2 weeks apart. The results support simultaneous administration of mRNA COVID-19 and inactivated influenza vaccines since no significant differences in aftereffects were observed. There are some limitations in the study since the study group only included small numbers of children, people over 65 years old, and pregnant people.
- The WHO reports that while mpox cases are rising across Africa, activity in one hotspot, South Kivu province in the Democratic Republic of the Congo (DRC), appears to be stabilizing. The novel clade 1b virus, present in six DRC provinces, has spread to 11 other countries, primarily through close contact among young adults, including sexual transmission. The virus is now increasingly affecting households, communities, and children. In Burundi, the outbreak is centered around Bujumbura, with similar patterns of transmission impacting young adults and children. Testing challenges continue to hinder a full understanding of the outbreak’s spread.
- Over the weekend, British Columbia officials reported a presumptive positive H5 avian flu infection in a teenager who is currently hospitalized. If confirmed, this would mark Canada’s first locally acquired case. Investigation is underway to determine how the patient was exposed.
- Rwanda discharged its last Marburg virus patient on November 8, beginning a 42-day countdown before the outbreak can be officially declared over, according to the WHO. No new cases have been reported since October 30, keeping the total at 66 infections, with 15 fatalities, making it the third-largest Marburg outbreak to date. Despite the decline, Rwanda continues active case finding to ensure no transmission chains were missed. The outbreak, declared in late September, was traced back to a patient who likely contracted the virus from bats near Kigali, with many cases involving healthcare workers and family members.