While the current assessment for the U.S. human health risk from avian influenza A (H5N1) remains low, CDC has created a “Risk by Exposure Table” in the appendix of their Avian Influenza interim recommendations page that categorizes people—such as farm workers or household members—by the degree of risk of infection based on their setting and exposure. Currently, the table focuses on cow-related exposures, but it will be updated in the future to also include bird-related exposures.
Among the groups listed, the highest relative risk for H5N1 infection is found in farm and slaughterhouse workers who have close contact with infected cows. CDC then ranks the risk of infection for the following groups as:
- High to medium risk: household members of person with confirmed or suspected H5N1 infection and workers on an impacted farm who have no direct contact with the infected cows. These workers could be exposed to the virus through contact with contaminated environment, animal waste, or water.
- Medium risk: Non-farm occupational exposures—which could occur through transportation, pasteurization plants, or milk testing laboratories.
- Medium to low risk: time-limited visitors to farms with infected cows who have no close animal contact, health care workers exposed to infected persons, and individuals exposed through non-farm recreational activities—such as fairs, livestock shows/auctions, petting zoos, and agritourism.
- Low risk: workers on a farm without infected cows. The risk increases for human infection if the animals appear healthy but are asymptomatic or pre-symptomatic.
Also included on the table are individuals who drink or are exposed to potentially contaminated raw milk from infected cows. CDC states the level of risk to humans is unknown but of high concern based on current animal data and testing. CDC and TAG advise against drinking raw milk because pasteurization is necessary to kill viruses in the milk, including H5N1.
In its most recent update, CDC also discusses the virus’ preference in infecting birds over humans. Studies on the A/Texas/37/2024 strain show the virus’ hemagglutinin surface protein bonded to host cells with avian-type receptors but not to those with human-type receptors. H5N1 has yet to adapt to better infect people, which is one reason CDC states the general public’s risk remains low.
As additional data becomes available, CDC will continue to assess risk and update their table and recommendations. As of now, CDC recommends avoiding exposure to sick or dead animals and to animal poop, litter, or materials that have come into contact with birds or other animals infected by H5N1 virus. Additionally, farmworkers or individuals who have job-related contact with infected animals or birds should take proper precautions, including wearing personal protective equipment.
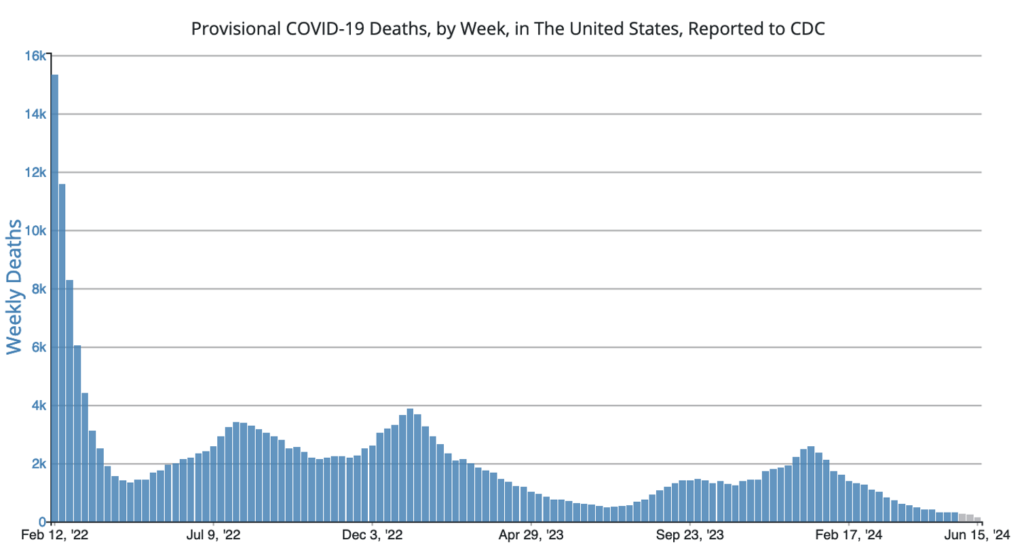
COVID Risk Matrix:
Influenza:

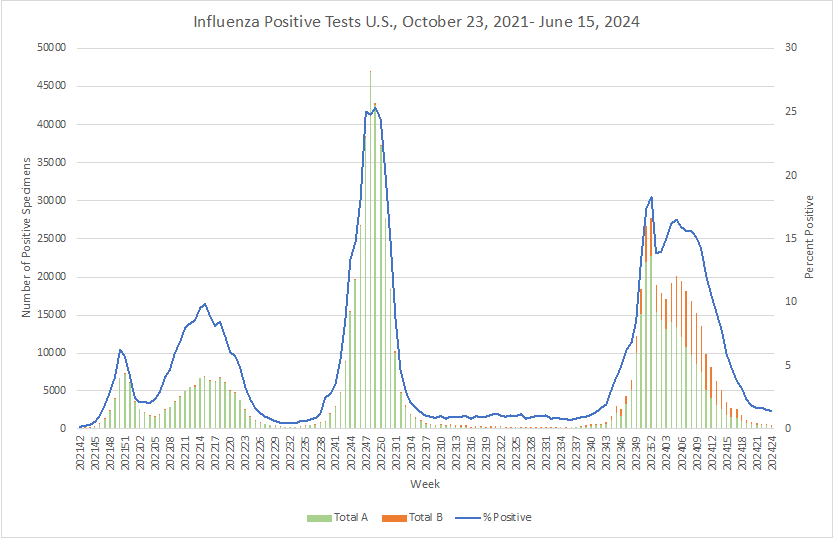
- In a study of 300 health care workers who received flu vaccines from 2019 to 2022 and the fall 2022 bivalent COVID-19 vaccine, women were more than twice as likely as men to report local adverse events after influenza or COVID-19 vaccination, with more disruptions in daily life.
- In 2024, The Government Service Agency began testing at many federal buildings to support the health and safety of those who work in and visit those buildings. Their testing revealed the presence of Legionella bacteria in the Lloyd D George federal courthouse in Las Vegas. Corrective and preventive actions are in progress. No illnesses have been reported.
- Cases of rare and potentially fatal meningitis bacterial infections are on the rise in Manitoba at a rate about 3x of what is typically reported. 19 cases of invasive meningococcal disease and 1 death have been recorded since December 2023. Since meningococcal bacteria can lay dormant in the back of the throat for many years and not cause problems, any emergence of rapid onset respiratory symptoms should be evaluated.
- Whooping Cough:
- Cases of whooping cough in Michigan are on track to be double last year’s rate and be back at the pre-pandemic rate.
-
- Rates of whooping cough are tracking 5x higher than the past couple years in Australia. There have recently been epidemics of pertussis there every three to four years. This normal cyclical pattern is due to waning immunity over time due to lack of exposure to circulating infection.
- Fayette County in KY continues to experience a whooping cough outbreak, part of a statewide year-to-year increase in cases of the disease that is most serious in infants, young children and those with chronic diseases. 27 cases are reported since late April, which is about 1.5x the normal rate.
- The USDA updated its case counts of H5N1-infected dairy herds last week, confirming 121 cases in 12 states since the beginning of the outbreak. There have been 58 confirmed cases in the last month, with Idaho reporting the most recent cases with 17 livestock herds affected in the past month.
- The US Administration for Strategic Preparedness & Response (ASPR) has outlined its strategy to tackle H5N1 avian flu infections in US cattle and poultry, following a new outbreak in Iowa. ASPR, part of the Department of Health and Human Services, is monitoring the situation and providing resources to support various partners. The Strategic National Stockpile (SNS) has personal protective equipment (PPE) and antiviral drugs like Tamiflu available, with additional materials for vaccines if needed. So far, three H5N1 cases in humans have been confirmed in the US in 2024. ASPR is also offering protective gear for farm workers and others in contact with infected animals.