Using an old technique that’s new again, MIT researchers have discovered a class of compounds that can kill methicillin-resistant Staphylococcus aureus (MRSA). Deep learning teaches computers to process similar to that of the human brain; it is able to recognize and provide insights and predictions from complex patterns (e.g., from graphics, text, sound, etc.).
MRSA infects more than 80,000 people, causes more than 10,000 deaths each year in the US, and is one of the greatest threats to human health globally. As one of the most difficult to kill pathogens, the infection causes skin lesions, which can lead to infection, pneumonia, or sepsis, which can be fatal.
The MIT research showed that the compounds were effective against MRSA grown in a lab dish and in two mouse models, and they have little toxicity against human cells. The use of AI was of particular interest in the study, because the researchers were able follow its reasoning to determine the types of date by which the model was making its antibiotic potency predictions. The deep learning showed “what was being learned by the models to make their predictions that certain molecules would make for good antibiotics.”
This is important because it could enable researchers to design other drugs that would work even better than those found through the study. The speed of the AI learning is also significant as it greatly reduces the time from discovery to market. Traditionally, it takes more than a decade to discover a new antibiotic and another several years to determine clinical candidates to run the clinical trials. The AI-guided discovery can also address the need for new novel antibiotics to address the growing issue of antibiotic resistance.
With the approach demonstrating that AI models in drug discovery can be explainable and provide insights into the chemical substructures that underlie selective antibiotic activity, the researchers are continuing their study with a goal of discovering new antibiotic classes against seven types of deadly bacteria within seven years.
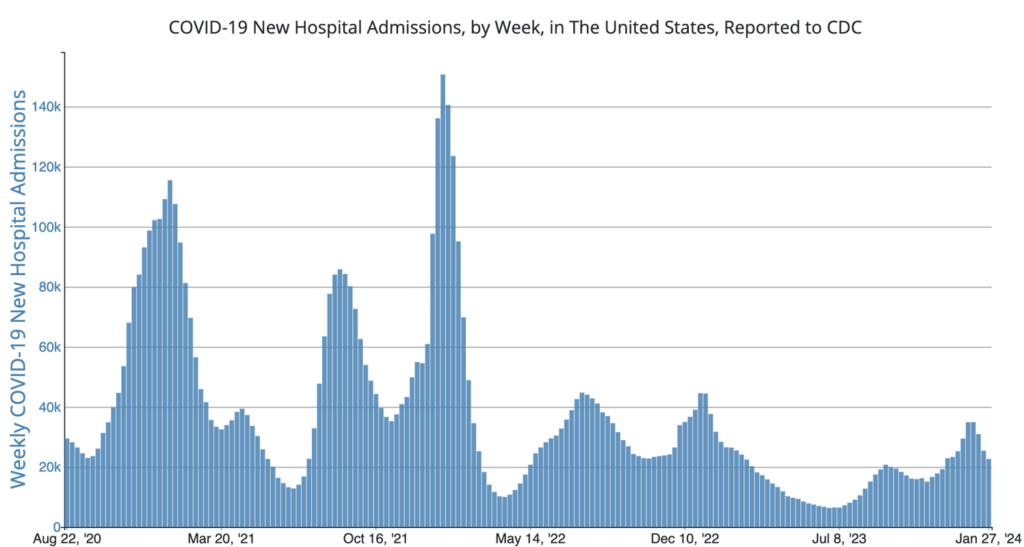
COVID Risk Matrix:
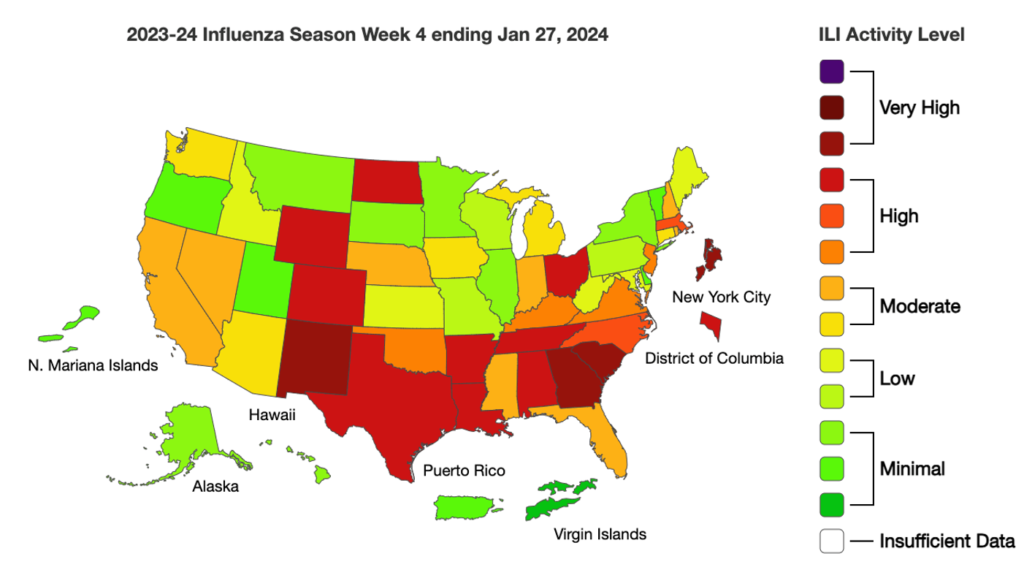
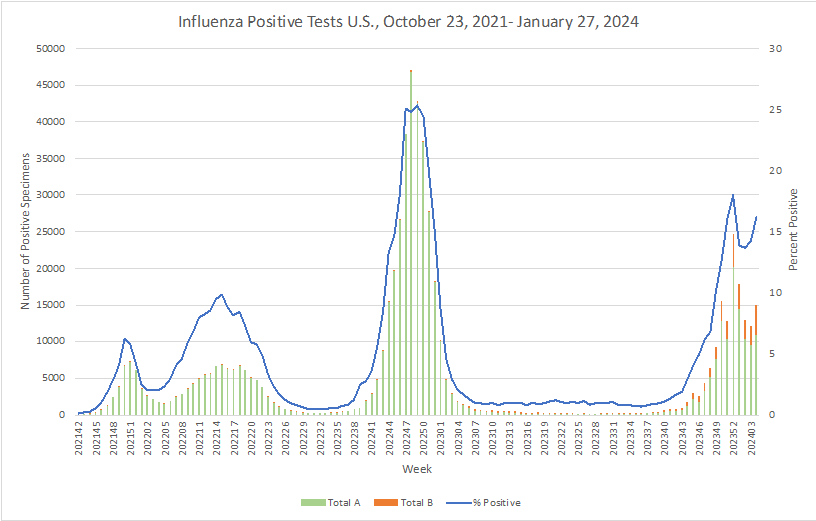
Influenza:
- Early estimates provided by the CDC of the updated monovalent XXB.1.5 COVID vaccine effectiveness against symptomatic SARS-CoV-2 infection is approximately 54%.
- Since the beginning of the school year, flu and COVID-19 data from 16 air monitors at 15 schools in or near Dane County, Wisconsin has been reported on a respiratory illness dashboard. The devices, roughly the size of microwave ovens, are placed in communal spaces such as cafeterias. Air (and the viruses it may contain) is drawn into spongy material that is analyzed for viral genetic material.
- The University of Pennsylvania’s School of Veterinary Medicine had developed techniques for lung repair after COVID or the flu, that deliver vascular endothelial growth factor alpha via lipid nanoparticles. This technique permits enhanced repair for damaged blood vessels in lungs.
- According to the CDC, around 11% of children, 21% of adults and 41% of seniors said they’re up to date on getting the latest COVID vaccine. Many more people get flu vaccines. Nearly half of surveyed children and adults got their shots, and more than 70% of seniors have received theirs. Reasons are not entirely understood but include confusing public health messaging from the media or the hassle of having to get two shots.
- Cases of invasive group A strep are rising across Canada. Provinces have reported dozens of deaths in just the last few months, including at least 10 children across Ontario and in B.C. The Public Health Agency of Canada suggests the current rate of infection could be as high as 12 cases per 100,000 people.
- Around one in five people develop cancer in their lifetimes, the International Agency for Research on Cancer found recently. Additionally, one in nine men and one in 12 women die from the disease.





