Although highly pathogenic avian influenza (HPAI) avian influenza outbreaks in poultry are continuing to be reported at commercial poultry farms in both the U.S. and Canada and globally, the threat to humans remains very low. Despite some sensational media headlines, only a small number of sporadic human cases have been identified since 2022, nearly all of which were associated with prolonged exposure to poultry.
The poultry outbreaks are certainly impacting that industry segment however, with a loss of nearly 80 million birds across 47 states since February 2022. The virus has been known to infect a wide array of wild birds and mammals, including foxes, skunks, mountain lions, sea lions, and most recently, a polar bear in Alaska. However, no cases of mammal-to-human or human-to-human transmission have been identified.
Additionally, CDC’s monitoring of more than 7,000 people in 52 jurisdictions who were exposed to infected birds or sick or dead mammals, about 175 were symptomatic, and only a single person tested positive for the virus. Those who work with or have recreational exposure to birds or infected mammals should protect themselves by:
- Minimizing contact with wild birds or sick or dead poultry by wearing gloves
- Washing hands with soap and water after touching birds.
- Wearing respiratory protection, preferably an N95 respirator if available, or a well-fitting facemask
- Avoiding touching the mouth, nose, or eyes after contact with birds or surfaces that may be contaminated with their saliva, mucous, or feces.
- Changing clothes before contact with healthy domestic poultry and after handling wild birds. Then, throwing away the gloves and facemask, and washing hands with soap and water.
Even for individuals with close proximity to birds, the potential of serious infection is very low because the currently circulating A(H5N1) virus cannot easily infect or transmit among people. Thus, despite its worldwide spread, only a small number of sporadic human infections have been reported since 2022, and no cases of human-to-human transmission have been identified.
For more information on Avian Flu, see TAG’s Infectious Disease Fact Sheet.
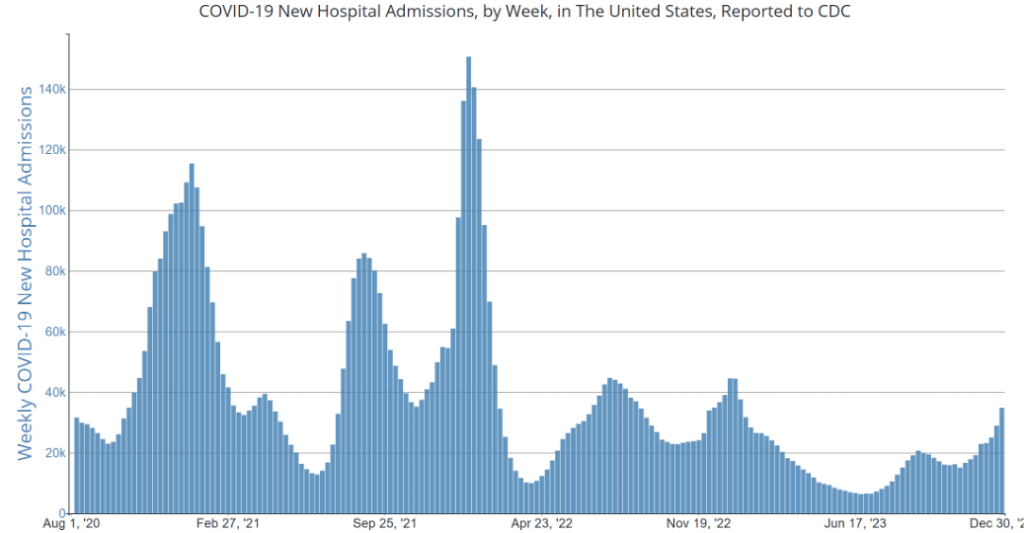
COVID Risk Matrix:
Influenza:
Infectious Disease News:
- As respiratory illnesses due to flu, Covid, or RSV continue to occur, precautions are being recommend; some health systems are reinstating mask mandates for patients and staff. Despite this, governments and businesses are not considering such mandates to date.
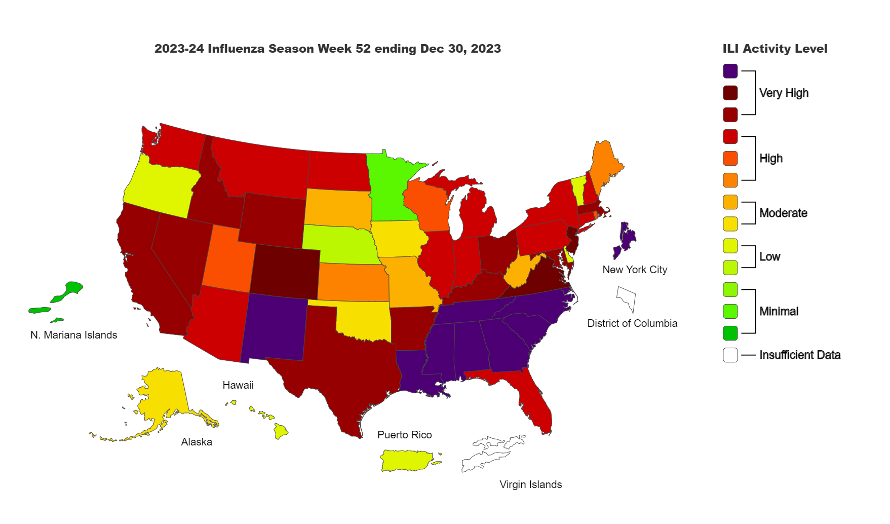
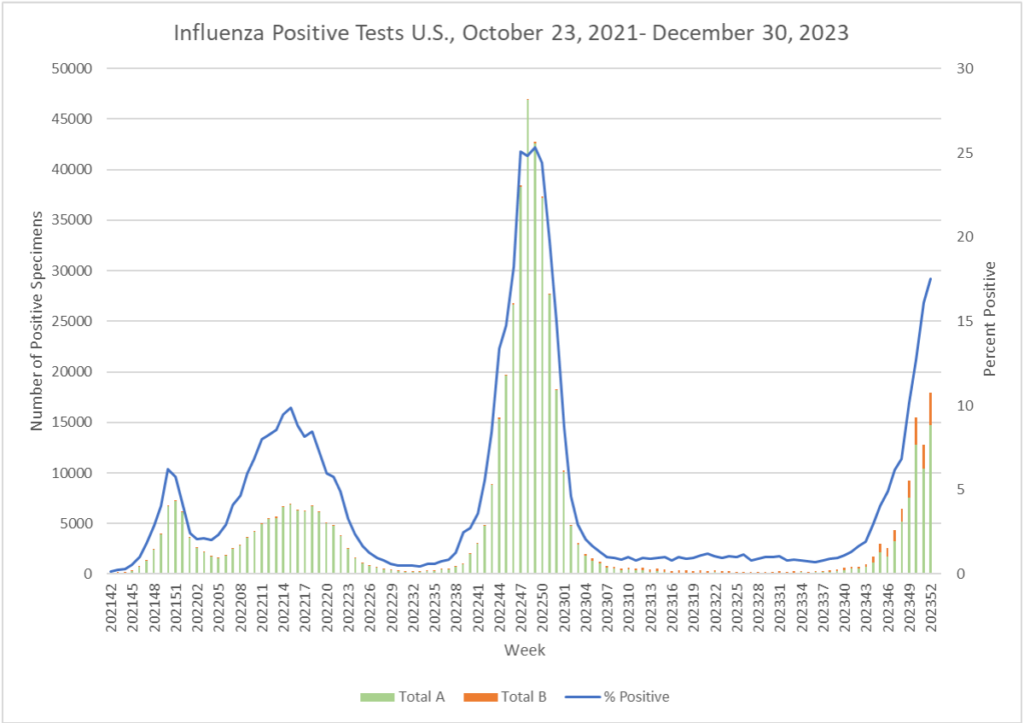
- Flu activity in the U.S. is increasing dramatically with high and very high activity levels seen throughout the country. Only four states (Minnesota, Oregon, Nebraska, and Vermont) have low flu activity levels. Flu hospitalizations and deaths have also increased.
- As respiratory infections also increase, pertussis is on the rise. New York’s Suffolk County Department of Health Services is tracking a growing number of pertussis cases, with the majority of the 108 cases in school-aged children (and their parents). The majority of patients were vaccinated so their illnesses were mild.
- Although we are seeing increased cases of avian flu, including isolated cases of avian influenza occurring in humans reported in China. One case was avian influenza A(H5N6) resulting in death, and two very mild cases were attributed to avian A(H9N2). These are likely related to zoonotic transmission. No human-to-human transmission has been reported. Overall risks to humans are deemed very low.
- A primer in a Ukraine news publication discusses how measles progression as more cases are being reported. Measles can incubate for up to 2 weeks; symptoms may manifest as high fever, red eyes, sore throat, headache, etc. On the 3rd-5th day of illness, a red, bumpy rash appears usually appear at the hairline and spread to the neck, torso, limbs, feet and arms. As it spreads, temperatures may begin to rise. Patients are contagious for 8 days – 4 days before and after the rash appears.
- There is news about Tuberculosis as well. In Indonesia, cases were seemingly down during the COVID pandemic, though that could be due to lesser surveillance, while in Poland, the current robust surveillance system seems to identify at least 90% of estimated TB cases. In Ireland, though, the bovine TB outbreak is being described as “the worst in years”.





