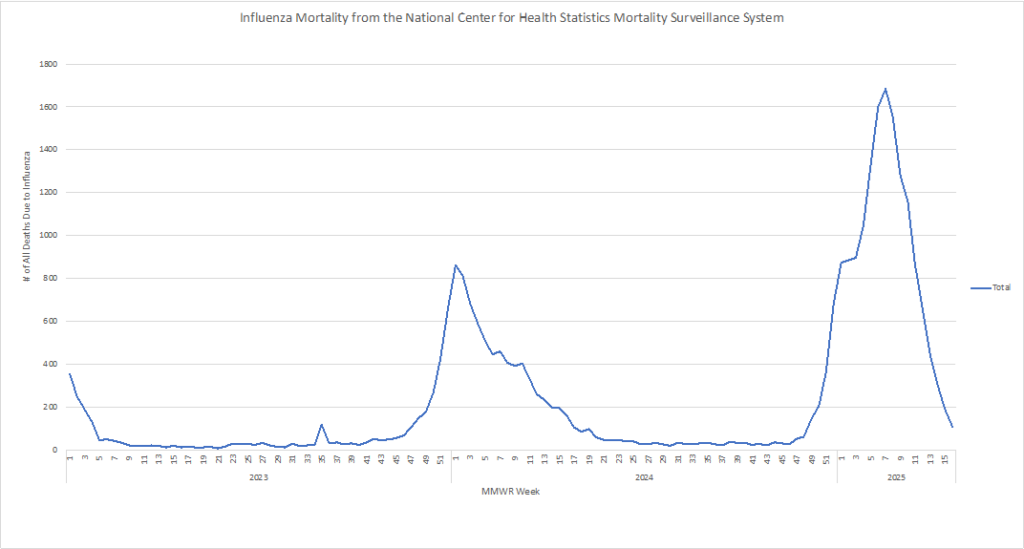
Although seasonal flu activity is declining with no new influenza A(H5) cases reported to CDC this week, the 2024-2025 season is classified as having high severity – the first since the 2017-2018 season. In total, there have been 216 pediatric deaths associated with influenza virus infection this season, which exceeds the previous high reported for a regular (non-pandemic) season, that occurred last season (2023-2024).
With CDC estimating that there have been at least 47 million illnesses, 610,000 hospitalizations, and 26,000 deaths from flu so far this season, the Center is recommending that everyone aged 6 months and older get an annual flu vaccine as long as influenza viruses are circulating.
To increase the transparency, effectiveness, and comprehensive preparedness of vaccine development, the HSS and NIH are working toward a next-generation “Generation Gold Standard” of universal influenza and coronavirus vaccines, which aims to provide broad-spectrum protection against multiple strains. Using a beta-propiolactone (BPL)-inactivated, whole-virus platform, the intention is to prepare for all influenza viral threats, not just those currently circulating. Unlike current vaccines, the new standard, developed by NIH’s National Institute of Allergy and Infectious Diseases (NIAID), preserves the virus’ structural integrity, while eliminating infectivity, and induces robust B and T cell immune responses to offer long-lasting protection and block virus transmission.
Being fully government-owned and NIH-developed, the approach is said to ensure transparency, public accountability, and freedom from commercial conflicts of interest. The platform is also adaptable for future use for respiratory syncytial virus (RSV), metapneumovirus, and parainfluenza, and can protect against avian influenza without inducing antigenic drift. Clinical trials for universal influenza vaccines are scheduled to begin in 2026, with FDA approval targeted for 2029.
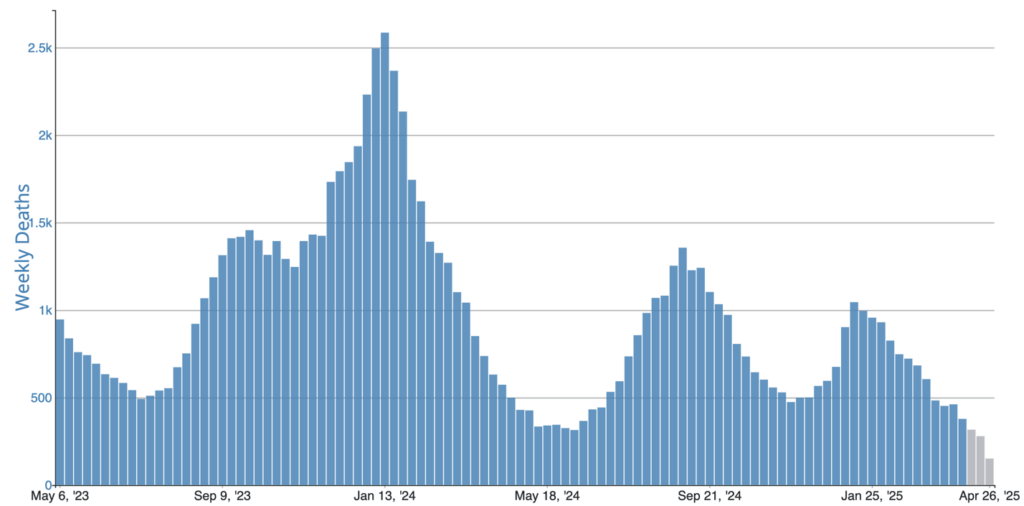
COVID Risk Matrix:
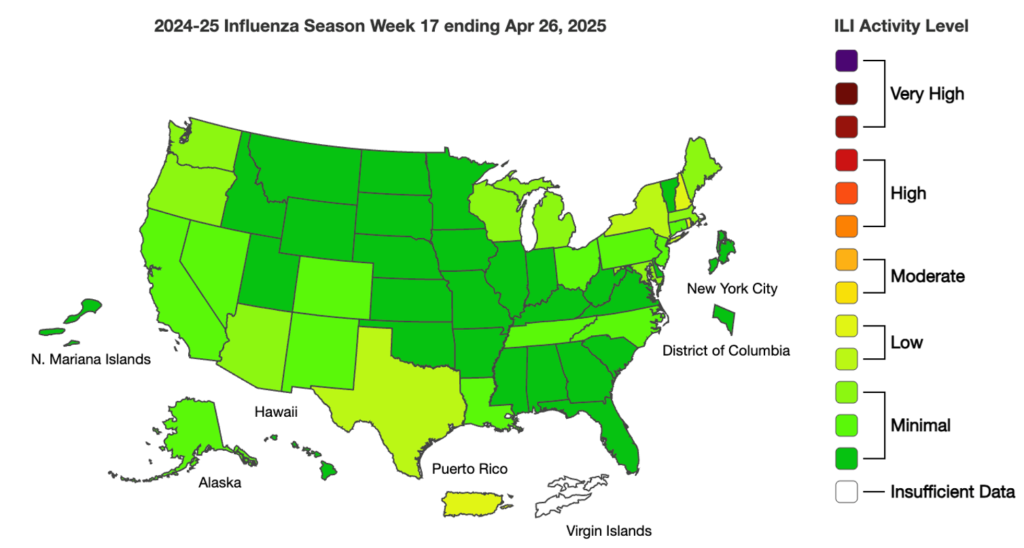
Influenza:
Infectious Disease News:
- The CDC has reported 54 new measles cases this week, bringing the national total to 935 across 30 states, with the majority linked to a large outbreak centered in West Texas. Texas alone accounts for 683 cases, most of which are in unvaccinated individuals. Health and Human Services Secretary Robert F. Kennedy Jr. has advocated for alternative treatments like vitamin A, but the CDC cautions against overuse due to toxicity risks and reiterates that vaccination remains the most effective protection. With summer travel and gatherings approaching, health officials are urging people to stay up to date on MMR vaccinations.
- The CDC has reported 12 additional pediatric flu deaths, bringing this season’s total to 216, the highest in a non-pandemic year. Most of the deaths were caused by influenza A, with the H1N1 strain being the most common. Overall flu activity is declining, with fewer outpatient visits and hospitalizations reported. COVID-19 and RSV activity remain low nationwide, though a few states are seeing higher levels of virus in wastewater.
- Louisiana is experiencing a significant rise in whooping cough (pertussis) cases, with 164 reported in the first four months of 2025; these numbers are surpassing last year’s total and have the potential to set a 35-year record. Most hospitalizations and both recent deaths have occurred in infants under one year old. The Louisiana Department of Health urges the public to review their vaccination status, practice good hygiene, and take precautions to protect vulnerable populations. Pregnant women are advised to receive the Tdap vaccine during each pregnancy to help protect newborns, who are at the highest risk, but cannot be vaccinated until two months of age.
- A new WHO report analyzing 2022 data reveals many countries are overusing antibiotics that drive antimicrobial resistance, with only 52% of antibiotic use falling into the recommended “Access” category. The Global Antimicrobial Resistance Use and Surveillance System (GLASS) data showed wide variation in antibiotic consumption, with some countries, like Iran, using nearly nine times more antibiotics than others. Most countries failed to meet WHO targets for Access antibiotic use, while overuse of broader-spectrum “Watch” antibiotics was common. The report also identified limited access to last-resort “Reserve” antibiotics in many low- and middle-income countries and emphasized the need for improved surveillance and responsible prescribing practices to combat rising resistance.





