Even as USDA announces new HPAI detections in animals and implements enhanced testing and monitoring, the current public health risk in the U.S. continues to be low.
In late October, the USDA confirmed that a pig on an Oregon backyard poultry and livestock farm was infected with H5N1, marking the first detection of the virus in swine in the U.S. Because the livestock and poultry shared water sources, housing, and equipment, when H5N1 was detected in poultry on the farm, the swine were tested as well. Only one of the five swine has, thus far, been found to be infected, as test results were negative for two and still pending for two.
With the farm being non-commercial, there is no concern about the safety of the nation’s pork supply as a result of the positive finding. But the farm has been quarantined to prevent further spread, and its other animals are under surveillance. Additionally, USDA genomic sequencing of the virus from the farm’s infected poultry does not suggest that it is more transmissible to humans, thus the current risk to the public remains low.
Meanwhile USDA APHIS is enhancing its testing and monitoring for H5N1, implementing a tiered strategy to collect milk samples to better assess where H5N1 is present. Working with regions and states, USDA plans to first sample milk in bulk at the regional level, then conduct testing at the farm level, when necessary, until herds in an area are determined to be free of the virus. USDA is working with state and private veterinarians on the final details of implementation and plans to share guidance documents soon.
Other steps that have been or are being taken include:
- Because H5N1 can be transmitted on equipment, people, or other items that move from farm to farm, a USDA Federal Order, announced in April 2024, requires testing before cattle movement between states.
- Farmers are encouraged to practice good biosecurity even if the virus has not been detected in their state or vicinity.
- USDA scientists, who work closely with those at the CDC and across the country, have not found any recent H5N1 changes that increase the risk of transmission from animals to humans or between people.
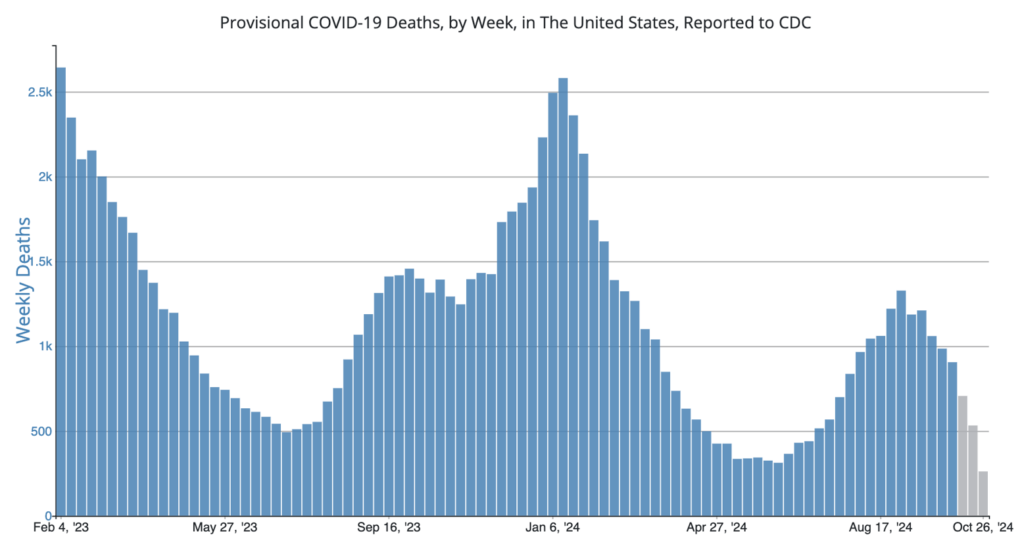
COVID Risk Matrix:
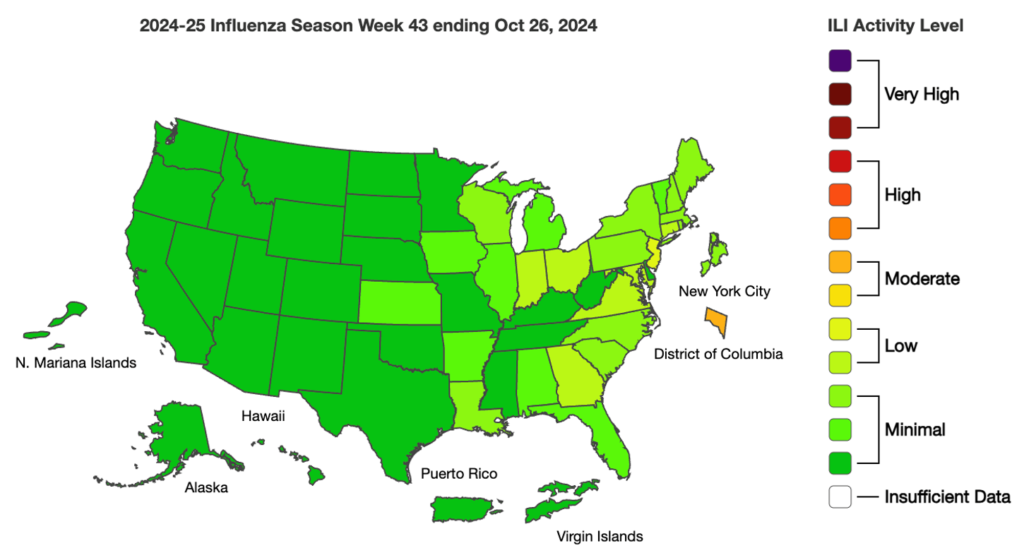
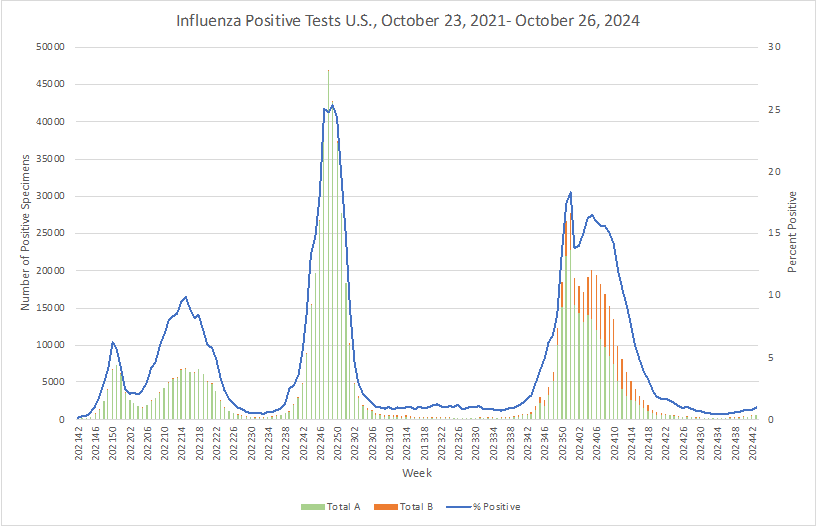
Influenza:
- In the UK, the number of norovirus outbreaks reported to the Hospital Norovirus Outbreak Reporting System since the start of the 2024/2025 season is 37% higher than the 5-season average.
- The World Health Organization published a new report on tuberculosis revealing that approximately 8.2 million people were newly diagnosed with TB in 2023 – the highest number recorded since WHO began global TB monitoring in 1995. According to the report, India (26%), Indonesia (10%), China (6.8%), the Philippines (6.8%), and Pakistan (6.3%) together accounted for 56% of the global TB burden and more than half of people who developed TB were men, one third were women, and 12% were children and young adolescents. Multidrug-resistant TB remains a public health crisis. Global funding for TB prevention and care decreased further in 2023 and remains far below target with low- and middle-income countries bearing 98% of the disease burden.
- Ethiopia is experiencing its worst malaria outbreak in 7 years, with more than 7.3 million cases reported since the first of the year, along with 1,157 deaths, the World Health Organization said in a notification. Plasmodium falciparum is responsible for two thirds of the cases.
- A research letter in the New England Journal of Medicine documents vertical (mother-to-baby) transmission of Oropouche virus (OROV) in Brazil this summer. The case resulted in the stillbirth of the baby, after the 40-year-old mother reported fever, chills, generalized muscle aches, and severe headache at 30 weeks’ gestation.